An Early Detection of Oral Potentially Malignant Disorders (OPMDs); Impact of Maxillofacial Surgeon-Led Biopsy Clinics. A Meta-Analysis and Systematic Review.
Oral Cancer is one of the main health issues that ranks among the top 10 most common cancers across the world. In this report “An Early Detection of Oral Potentially Malignant Disorders (OPMDs); Impact of Maxillofacial Surgeon-Led Biopsy Clinics. A Meta-Analysis and Systematic Review”, we explain Oral Potentially Malignant Disorders (OPMDs) and its treatment. The World Health Organization (WHO) estimated that almost 377,000 new cases of lip and oral cavity cancer were directly reported across the globe in 2020. WHO also examined that the oral space was linked to more than 177,000 associated deaths around the globe.
The majority of the cases are diagnosed in LMICS- Low and Middle-Income Countries, where the disease is often detected at the advanced phase, resulting in poor performance and success of limited treatments. A biopsy is a process in medicine where tissue or cells are removed from the body for examination. OPMDs- Oral Potentially Malignant Disorder is a critical challenge in oral cancer management with its frequent professional form of the existing conditions. Oral Potentially Malignant Disorders OPMDs indicate the clear spectrum of clinical presentations that carry the risk and transform into the OSCC- Oral Squamous Cell Carcinoma.
Common OPMDs refer to Leukoplakia, Oral Lichen Planus, and Erythroplakia. All of these conditions are often asymptomatic in the early phases and may be examined by non-specialist clinicians. Histopathological examinations through the biopsy can remain the gold standard for OPDMs’ diagnoses and assess the malignant potential. Patients may encounter delays with the fragmented referral pathways and the limited availability of some specialized diagnostic facilities.
There has been a rising interest in the development of Maxillofacial Surgeon-Led Biopsy Clinicians to fill this gap. Moreover, the involvements of Maxillofacial surgeons ensure that all the patients receive not only diagnostic services but also the appropriate surgical intervention with referral as needed.
Read more: The importance of applying managerial theories and practices in the health service sector
Problem Statement – Oral Potentially Malignant Disorders:
Significant batteries that persist in the current healthcare delivery frameworks, despite the recognized importance of early detection of Oral Potentially Malignant Disorder. Many patients are facing long waiting times for their oral lesion face surgeries, due to the inadequate referral system and the limited access to histopathological services.
Some general dental practitioners may not always have the key expertise to identify the Oral Potentially Malignant Disorders OPMDs, leading to delayed diagnoses. Furthermore, in various Healthcare Systems, the process of referring patients from primary care to the entire specialists can be inefficient or time-consuming.
Delayed scheduling of biopsies and initiating the treatments can result in disease progressional. Traditional models of care are not fully successful in addressing these delays. Clinicians should develop streamlined and multicollinear approaches that enable the rapid biopsy and diagnosis of oral lesions.
Research Question:
- What is the impact of maxillofacial subregion-led biopsy clicks on the early detection, management, and diagnosis of Oral Potentially Malignant Disorders?
Rationale for Study:
The increasing burden of oral cancer and the well-documented importance of Oral Potentially Malignant Disorder in the pathogenesis have raised early detection as a Public Health Priority. Multiple national as well as international cancer control strategies emphasize early diagnosis or screening, with the practical implementations that remain inconsistent. Maxillofacial surgeons develop the socialized turning in the Oral Pathology, Oncology, and the surveys that play a central role in the early detection strategy. Professionals who provide diagnostic services and contribute to care that enables patients to receive the surgical excision and counseling are the people who lead the biopsy clinics.
The global prevalence of Oral Potentially Malignant Disorders OPMDs was reported in India to be 1 to 5%. The incidence rates of oral cancer were highest in Malaysia and South Asia. Biopsy clinics can offer the same-day biopsy and reduce the anxiety of patients with the acceleration of treatments. Moreover, biopsy clinics can serve as a valuable portal for education and research. These clinics can also serve as the training it’s for dental students, healthcare professionals, and general dentists to recognize and manage the Oral Potentially Malignant Disorder. The rates were higher in Papua New Guinea at 21.2%, followed by Pakistan at 10.1%, India at 9.8%, Bangladesh at 9.5%, and Sri Lanka at 9.7%.
Significance:
The main goal of this research is to assess the entire contribution of the maxillofacial subregional biopsy to improve the management and early detection of Oral Potentially Malignant Disorders. The study is significant for various reasons. First of all, it analyzes the Critical Gap in the literature related to the role of specialist-led services in the presentation of oral cancer. Secondly, the study focuses on Specialist-Driven Intervention with information on national oral health policies. Third, the study may help to raise the outcomes for higher-risk populations and promote the models of care as both efficient and Patient-Centered.
Literature Review:
Overview of OPMDs (Oral Potentially Malignant Disorders):
Oral cancer is often preceded by a group of conditions known as Oral Potentially Malignant Disorders. OPDS are lesions and abnormalities in the mouth that carry the risk of becoming cancer over a specific time. Leukoplakia and Erythroplakia are the most common types of leukoplakia. All of these conditions are not only cancers, but they have the potential to transform the oral squamous cell carcinoma if not identified and treated. Early detection is crucial because it offers the window of opportunity to prevent the development of oral cancer. Multiple OPMD conditions are painless and appear as a subtle change in the oral lining, which can go unvoiced, but the patients ‘ general practitioner.
Challenge in OPMDs’ Early Identification:
Early detection of Oral Potentially Malignant Disorders plays a crucial role in preventing the progression to oral cancers. Moreover, in real-world clinical practices, multiple lesions are diagnosed only after they have transformed.
- One of the primary barriers to early diagnoses of Oral Potentially Malignant Disorders is the Lack of Awareness among the public related to oral health, as well as the warning signs of the conditions. Most OPMDs, like oral submucous and leukoplakia, begin as painless and subtle lesions.
These symptoms are not linked with the discomfort; patients often dismiss them as temporary issues. Moreover, people with low literacy levels or those from an economically disadvantaged background may lack access to oral health education. Lack of public health campaigns and oral cancer awareness contributes to the delays in seeking care. There were 3.5 billion cases of lip and oral cavity cancers that appeared all over the world. Higher incidence occurred in Melanesia, South-Central Asia, and the European parts.
- Biopsy Hesitations and lack of access to diagnostic services are another challenge that is facing their entire values. Biopsy remains the partitioners and primary healthcare provider that is typically the first point of contact for individuals with oral lesions. Many dental practitioners are not licensed or trained to perform medical treatments such as biopsies.
Some dentists may feel uncomfortable performing the biopsy due to the fear of complications like bleeding, infections, and patient dissatisfaction. There is a long waiting time for specialist appointments, which leads to further delays as patients never follow through with the referral due to fear. There were nearly 389,846 new cases of oral and mouth cancers that appeared globally in 2022, especially among contribute with the highest average rates.
The Role of Biopsy in Early Diagnosis:
A biopsy is one of the simplest and most powerful tools that allows clinicians to look at the tissue under the microscope and determine whether eh lesion is being, potentially malignant and already cancerous. Histopathological results from the biopsy also help to classify the degree of dysplasia, as a measure of how abnormal the cells are. Unfortunately, due to the various reasons mentioned earlier, access to biopsy services is inconsistent in the public healthcare system and low-resource settings. Many patients only undergo biopsy when the lesion becomes suspicious as well as painful, by which time it may already be too late for the cancer.
Maxillofacial Surgeon-Led Biopsy Clinics:
Maxillofacial surgeon-led biopsy clinics are being introduced as a new model of care in multiple biopsy clinics. These clinics are known as specialized declines as run by oral and maxillofacial surgeons, as experts are trained in diagnosing and treating the mouth, face, and jaw disease. Patients can be referred to the specialist clinics without going through various layers of referral. Patients can even self-refer, but the general public immediately refers to the clinics.
Maxillofacial SURGEONS have extensive training in oral pathology. Maxillofacial surgeons can evaluate the suspect lesions more accurately and perform immediate biopsies with the interpretation of clinical signs that generalists might miss. Patients can be examined on the same day, and this activity reduces the waiting period and speeds up the diagnoses, which is critical for improved outcomes. Maxillofacial surgeon-led biopsy clinics also served as centers of the same clinics that provide the surgical treatments and remove the lesion of the patient for cancer care.
Impact on Early Detection Rates:
There is a higher rate of identification and diagnosis of Oral Potentially Malignant Disorders are the earlier stages with more specialists. Clinics led by the maxillofacial surgeons have ended up performing more biopsies, leading to more accurate diagnoses and less guesswork. The traditional referral system may take several weeks to months; specialized clinics provide the results within days. Lesions are diagnosed early, with the treatment sis simple and less invasive, with more successful results.
Patients who attend specialist biopsy clinics report higher satisfaction due to short wait times, better communication with the knowledgeable professionals, and more confidence in diagnoses. Notable countries that have higher rates of oral and mouth cancers are Papua New Guinea, India, Pakistan, and Bangladesh.
Barriers and Solutions to Wider Implementation:
There is a limited number of maxillofacial surgeons, underserved areas and rural areas. Cost and resource constraints are another major barrier that prevents business activities from achieving the desired results. Maxillofacial surgeons may still struggle to access the centralized specialist clinics.
Biopsy clinics should enhance the training of general practitioners to recognize the OPMDs and perform the basic biopsies where specialists are not available. These clinics should educate the public on the importance of early oral lesion detection and encourage routine oral screening. Maxillofacial surgeon-led clinics in the cancer prevention strategies that allocate the resources for the broad development and entire areas of success.
Application of Andersen’s Behavioral Model to Early Detection of Oral Potentially Malignant Disorders:
Andersen’s Behavioral Model of Health Services Use is a popular framework used to examine why people use healthcare services. Andersen’s Behavioral Model helps to explain which factors influence individuals’ decisions to seek medical care and how the healthcare activities.
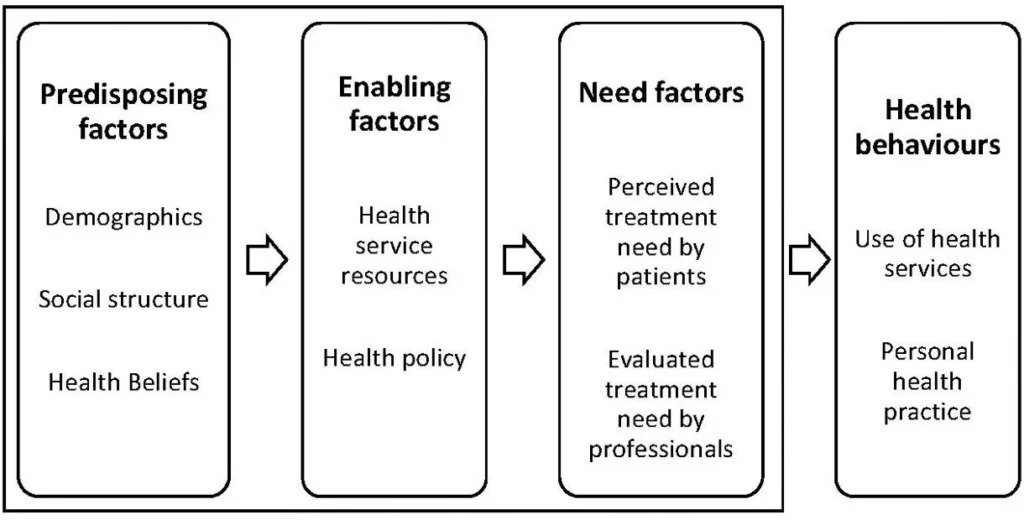
Predisposing Factors:
Predisposing factors are the personal characteristics that make someone more and less likely to seek healthcare. Many people don’t recognize the early signs, like modules and white patches, which are not dangerous unless painful. Adults, especially those who use alcohol and tobacco, are at higher risk but may not be aware of the risk. People with low education or health literacy may not understand what OPMDs are and when they should be examined.
Enabling Factors:
Enabling factors are practical resources and barriers that help prevent people from accessing healthcare. Patients in rural as well as low-income areas may not have clear access to dentists trained in identifying the OPMDs. Higher cost of private clinics and long distance to the hospital can limit the follow-up services. Maxillofacial surgeon-led biopsy clinics help to remove the barriers by offering direct care in one place.
Need Factors:
Many OPMDs don’t cause pain at first, so patients may not feel the need to seek help. If penitents don’t trust the entire advice, it helps the patients to understand and importance of early actions. Oral cancer continues to be a serious issue of health issue, especially in countries with limited access to healthcare . OPMDs offer the critical opportunity to integrate early and before the cancer develops. Moreover, developments in diagnoses remain common due to the gaps in awareness, access, and training.
Maxillofacial surgeon-led biopsy clinics offer a promising solution by offering expert, timely, and streamlined care. Challenges remain in executing of model and in low-resource settings, with the impact on public health as significant roles. Future research must be focused on evaluating the clinic’s effectiveness and systemic change that the health system can adapt or expand the models where it is needed most.
Methodology:
The study explores the impact as well as the role of the Maxillofacial surgeon-led biopsy clinics in the early detection of Oral Potentially Malignant Disorders. The study focuses on how all of these clinics contribute to better diagnostics and patient outcomes with the system efficiencies. Research is designed as a qualitative study based on secondary data. Research refers to the collection of new data through surveys and interviews with the relies on current information like reports, published studies, and expert opinions.
Design:
The study designs are descriptive and explanatory qualitative research, as it does not aim to test the hypotheses through numerical measurements but rather to explore the times, experiences, and the factors related to system-related issues. The study describes the structure and workflow of maxillofacial biopsy clinics and highlights the patient outcomes. No patients or clinical procedures are involved directly in the study, as observations are drawn from the current study.
Data Collection:
Data used in this study comes from a range of secondary sources. Public peer-reviewed articles, clinical audits, institutional reports, case studies, professional commentaries, global health databases, and government and NGO policy documents are some data sources that help to collect the data and gather the most relevant information related to the entire data. WHO- World Health Organization and Global Burden of Disease Study, relying on national cancer registries.
Inclusion and Exclusion Criteria:
The data collection process involves different steps, like database search, inclusion criteria, and exclusion criteria.
Inclusion:
Studies or reports that focus on the diagnosis and management of Oral Potentially Malignant Disorders are involved in this research. Publications that refer to the data on diagnostic timelines and patient satisfaction are also involved in this entire data. An article that discusses the specialist-led clinics in the oral as well as maxillofacial sure they are also be involved in this broad term.
Exclusion:
Studies focusing only on the treatment of advanced oral cancer without discussion of early detection. Articles that are not related to biopsy procedures and the specialist clinics are also not involved in this research. The duplicated and low-quality data without any pre-review are not linked to the data for this study.
Data Analysis:
Secondary sources are used to collect the data, but the data can be analyzed in the form of results gathered from multiple studies. Meta-analysis and Systematic Review a process that are used to analyze the data. Data is examined from the number of independent studies on the same subject under the meta-analysis. Articles or studies related to the OPMDs and the maxillofacial Studies are used to review the systemic operations and meta-analysis within this research.
Thematically, the data is collected with familiarization and coding. Oral Potentially Malignant Disorders’ early detection for the biopsy clinics carefully reading the selected literature to gain a comprehensive understanding, comparing the findings from the different sources to identify the commonalities and fill the gaps in different plans. Syntheses and interpretations are the narrative roles that allow drawing the logical conclusion and bora implications.
Ethical Considerations:
This research is based entirely on secondary data, and there is no ethical approval from the institutional review board was required. No patient interviews, clinical trials, or personal data were collected. The article gives the sources through proper referencing and avoids the misrepresentation of data that is not related to the entire study. The study uses a structured and qualitative approach based on secondary sources to explore the effectiveness of maxillofacial surgeon-led biopsy clinics in the earlier detection of the Oral Potentially Malignant Disorders.
Results:
Oral Potentially Malignant Disorders were higher in different regions according to the data that had already appeared in the past. Oral cancer becomes increase across the globe year to year due to the lack of awareness of the people about the actual diseases and the less efficiency of the ways that decrease the cleared resources Papua New Guinea has the rate of Oral Potentially Malignant Disorders about 21.25%, Pakistan has the rate of Oral Potentially Malignant Disorders as 10.1%, India also has the 9.8% rate of Oral Potentially Malignant Disorders.
On the other hand, Bangladesh has a rate of 9.5%, and Sri Lanka has a rate of 9.7%. There is a strong need for biopsy clinics that help to raise awareness about oral and maxillofacial surgery to protect he cancers and decrease the overall death rates. Data underscore the political contributions as an important part of proteasomal advocacy and understanding the partners to inform the supercilium organoiron.
Nonpartisan, Democrat, and Republican are the political categories that classify the entire sources for the awareness and contribution the cancer-based activities. This graph shows the total political contributions to oral cancer across the world. In 2020, the oral cancer rate was high that leading to deaths due to a lack of awareness among people about how to manage it and ways to protect their lives from this.
The study highest the political engagement of the oral as well as maxillofacial surgeons in the United States, focusing on the frequency, amounts, and geographic distributions. OMD professionals are active political donors and contribute nearly 5 million Dollars across the 21799 donations, which were made but the 4,000 individuals. The patterns suggest a stronger realignment of the specialty with the Republican ideals and policy preferences regarding taxation and private healthcare. Democratic contributions still represent the meaningful subsets of OMD donors and indicate the ideological diversity within the field.
| Rank | Country | New Cases | Age Standardized Rate / 100,000 |
| World | 389,846 | 4.0 | |
| 1 | India | 143,759 | 9.9 |
| 2 | China | 37,208 | 1.5 |
| 3 | United States | 27,750 | 4.6 |
| 4 | Bangladesh | 16,083 | 10.3 |
| 5 | Pakistan | 15,915 | 9.2 |
| 6 | Japan | 11,088 | 3.1 |
| 7 | Brazil | 11,029 | 3.8 |
| 8 | Russia | 9,729 | 3.9 |
| 9 | France | 7,195 | 5.6 |
| 10 | Indonesia | 6,515 | 2.2 |
Mouth and Oral cancer rates increase from year to year. Table 1 shows the mouth and oral cancer rate from year 2022, according to age standardizations. There were 389,846 people as new cases that affected by mouth and oral cancer across the globe, with the age-standardized rate of 4.0. India has 143,759 new cases, China has 37,208 new cases, and Japan has 11,088 new cases of mouth and oral cancer with different ASR- Age Standardized Rate.
| Rank | Country | New Cases in Men | Age Standardized Rate / 100,000 |
| World | 268,999 | 5.8 | |
| 1 | India | 107,812 | 14.7 |
| 2 | China | 24,169 | 2.0 |
| 3 | United States | 18,901 | 6.6 |
| 4 | Bangladesh | 10,785 | 12.1 |
| 5 | Pakistan | 10,745 | 12.1 |
| 6 | Japan | 8,269 | 6.3 |
| 7 | Brazil | 6,596 | 6.5 |
| 8 | Russia | 6,545 | 4.3 |
| 9 | France | 4,737 | 8.3 |
| 10 | Indonesia | 4,010 | 2.9 |
Both men and women are affected by mouth and oral cancer across the globe. There was a total of 268,999 men that affected by mouth and oral cancer diseases across the globe. In India, 107,812 men had mouth and oral cancer in 2022, China had 24,169 new cases of oral cancer in men at year 2022, and Japan had 8,269 new cases of mouth and oral cancer in 2022.
| Rank | Country | New Cases in Women | Age Standardized Rate / 100,000 |
| World | 120,847 | 2.3 | |
| 1 | India | 35,947 | 5.0 |
| 2 | China | 13,039 | 1.0 |
| 3 | United States | 8,669 | 2.7 |
| 4 | Bangladesh | 5,298 | 6.9 |
| 5 | Pakistan | 5,170 | 6.2 |
| 6 | Japan | 4,543 | 1.9 |
| 7 | Brazil | 3,133 | 2.0 |
| 8 | Russia | 2,760 | 1.6 |
| 9 | France | 2,505 | 1.6 |
| 10 | Indonesia | 2,458 | 3.1 |
Table 3 shows that women also suffer from mouth and oral cancer across the globe. There was a total of 120,847 new cases appear within women that affected by mouth and oral cancer across the globe in 2022. India had 35,947 new cases of mouth and oral cancer within women, and China had the rate of ASR 1.0 with 13,039 new cases of mouth and oral cancer within women, in the year 2022. Japan has 4,543 new cases of mouth and oral cancer in women as of 2022.
Papua New Guinea, Bangladesh, India, Pakistan, and Sri Lanka are the main top 5 countries that have the highest cases of mouth and oral cancer in 2022. Papua New Guinea had an ASR of 17.5 in 2022, which refers to one of the top countries that faced the mouth and oral cancer new cases in 2022.
Discussion:
Based on meta-analysis and systematic review, the research article explores two interlinked but different themes. First of all, it examines the widespread burden of OPMDs- Oral Potentially Malignant Disorders in the higher-risk regions like Papua New Guinea, Pakistan, Sri Lanka, and others. Secondly, the article investigates the political engagement of oral as well as maxillofacial surgeons in the United States, examining the patterns of political contributions and how these may shape health policy.
OPMDs prevalence data paint a stark picture, with the higher rates of Papua New Guinea at 21.25%, India at 9.7%, and Bangladesh at 9.5%. These rates underscore how common oral lesions that may become caseous and unaddressed are in populations with limited resources. Biopsy clinics are reworked to raise awareness among the people related to oral cancer and maxillofacial surgeries to prevent the entire practices. Consistent with the literature in the field also supports the continuity of care and encourages the patients to follow through the entire treatment plan. Convergence of awareness and access sis a key to tackling the OPMDs prevalence. Biopsy clinics should initiate the proper campaigns for the early detection of Oral Potentially Malignant Disorders.
These campaigns have involved the traditional communication channels like radio, community health workers, and the risk factors of timely evaluations. Based on the clinical side, strengthen the diagnosis capacities of the top and front-line providers in terms of recognizing suspicious lesions are referring the patients quickly. Maxillofacial surgeon-led biopsy clinics distributed or supported by the mobile units in the remote areas. OPMDs are evaluated and managed properly with further research, which helps to improve the quality or refine the regional strategies.
Table 1 shows that the new cases of mouth and oral cancer across the world affect the health sector and the entire operations of the countries. There was a total of 389,846 new cases of mouth and oral cancer that appeared in the global market, with the ASR rate of 4.0. Indonesia has a lower rate, with about 6515 new cases, and Russia had 87,29 cases. And India has a top rate of about 143,759 new cases. So, there is a strong need for OPMDs and Maxillofacial surgeon-led biopsy clinics, which help to control this rate by early detection of the diseases.
Table 2 indicates the overall cases of mouth and oral cancer that are faced by men across the globe. India has the top country where most of the cases are suffered by men, like 107,812, with an ASR of 5.8. There is a strong need for early detection of OMPDs that helps to coordinate the disease and give the proper verification with the treatments to the affected patients. Maxillofacial surgeon-led biopsy clinics first initiate their early detection operations in India because it has a higher rate of mouth and oral cancer, which leads to the death of people.
Table 3 indicates the women who were affected by mouth and oral cancer in 2022. Brazilian women had 2760 new cases of mouth and oral cancer in 2022; Chinese women had 13,039 new cases, and Indian women had 35,947 new cases. So, there is a so a strong need to initiate the Maxillofacial surgeon-led biopsy clinics for the early detection of OPMDs- Oral Potentially Malignant Disorders.
Political parties also contribute to detecting the Oral Potentially Malignant Disorders and build multiple biopsies clinics across small over the world to protect against the higher rates of OPMDs. From 2013 to 2022, OMD professionals developed almost 21.799 contributions in which republican, nonpartisan, and democratic contortions are involved. So, these patterns suggest a stronger alignment with the coordinated and private-sector policy on taxation and clinical autonomy. Political donation data is specific to the United States and offers broader insights, with professionals in oral health able to participate in the political insights as relevant across borders.
Professional associations are politically informed and effectively lobby for better oral services. Surgeons and associations can advocate for the reduction campaigns and support the entire public health messaging with the support of awareness in high-risk communities where OPMDs are widespread. Encouraging research infrastructure and political engagement could lead to higher funding for data collection and prevalence in the regional hotspots.
Conclusion:
The research has explored the public health issue of OPMDs- Oral Potentially Malignant Disorders in their increasing global prevalence through early detection and timely treatments. Oral Potentially Malignant Disorders have various forms like erythroplakia, leukoplakia, and lichen planus, with the oral submucous as a warning sign that may lead to oral cancer. Literature review revealed that the biggest barriers to early diagnosis are low to analyze public awareness, inadequate training, and primary healthcare.
Many dentists are not confident or trained to perform the biopsies, and patients are referred to specialists, which leads to more delays. Maxillofacial surgeon-led biopsy clicks have been proposed and introduced into some healthcare systems. Patients in these clinics receive faster care and better follow-ups to improve outcomes and satisfaction. There is a strong need for biopsy kits that help to early detect Oral Potentially Malignant Disorders and oral cancers within the global market.
This research also explored how the political engagement by the maxillofacial and oral surgeons in the US reflects the influence on the entire policy of healthcare policy. The research highlights the higher risk of oral cancer, which is initiated with early detection of Oral Potentially Malignant Disorder. The study has significant operations to reduce the burden of oral cancer and improve patient outcomes across the world.